-
Programs & Courses
- Programs
- Courses
- Study
- Explore
-
Discover
- University Transfer
- Distributed Learning
-
Continuing Studies
- Upcoming courses
- StrongerBC future skills grant
- Small Business Essentials Micro-Credential
- Office Careers Essentials
- Esthetics
- Nail Technician
- Ed2Go Online Courses
- Ed2Go Online Career Programs
- Online Industry Safety Certifications
- Career & Professional Development
- Computer Skills
- First Aid, Health & Safety
- General Interest
- Industry Training
- Outdoor Recreation & Safety
- Service & Hospitality
- Trades
- English Pathway Program
- MS Office Certificate
- Equity and Accessibility in the Workplace Series
- Contract Services
- Publications
- International
- Admissions
-
Registration & Records
- Register for classes
- Register for Field Schools
- Register for Continuing Studies
- Grading policies
- Schedule Contract Services
- Tuition, fees & payments
- Refunds
- Student self-service
- Course schedules & important dates
- Request transcripts
- Request enrolment letter
- Graduation & credentials
- Forms
- Contact an advisor
-
Student Services
-
Student support
- Orientation
- Academic & accessibility supports
- Advising Services
- Indigenous student support
- Financial Aid
- Health & wellness
- Leaders in Action
- Community resources
- Campus services
- Library
- Safety & reporting
- Students' Union
- Careerhub
- Graduate resources
- Digital Ambassador Program
-
Student support
- Indigenous Resources
-
About CMTN
- About
- Campus locations
- Campus spaces
- Policies & procedures
- Accessibility at Coast Mountain College
- CMTN Foundation
- Board of Governors
- Education Council
- First Nations Council
- Centre of Learning Transformation (COLT)
-
Department contacts
- Accessibility Services
- Administration
- Admissions & Registration
- Ancillary Services
- Applied Coastal Ecology
- Business Administration
- Campus Store
- Career & College Preparation
- Centre of Learning Transformation (COLT)
- CMTN Foundation
- Communications
- Coordinators
- Culinary Arts
- Daycare
- Deans
- Directors
- Early Childhood Care & Education
- Educational Advisors
- Facilities
- Finance
- Faculty
- First Nations Access
- Food Services
- Freda Diesing School of Northwest Coast Art
- Health Programs
- Housing
- Human Resources & Payroll
- International
- Learning Assistance
- Library
- Link to Employment and Academic Pathways (LEAP)
- Management
- Northern Collaborative Baccalaureate Nursing
- President's Office
- Registrar's Office
- Registration
- School of Exploration & Mining
- Security
- Social Service Worker
- Student Records
- Student Services
- Trades
- University Credit
- Vice Presidents
- Warehouse
- Workforce Training & Contract Services
- Workforce Training
- News & media
- CMTN Careers
- Alumni Connections
- Footer
- Awards, Bursaries & Scholarships [DO NOT DELETE]
- Schedules & dates
- Library
- myCMTN
- Search result
- Campuses
- Terms of use
Overdose Prevention and Response at Coast Mountain College
In August 2024, the Ministry of Post-Secondary Education and Future Skills, in collaboration with BC post-secondary institutions, released a set of guidelines to help post-secondary institutions develop and implement an overdose prevention and response plan specific to their institution.
Since then, Coast Mountain College (CMTN) has been implementing these provincial guidelines on campus.
Why do we need an overdose prevention and response plan at CMTN?
In 2016, British Columbia declared a public health emergency in response to a significant increase in drug-related overdoses and deaths1. Since then, more than 15,000 lives have been lost in BC as a result of toxic drugs1 and, since the beginning of 2024, an average of six people die every day in BC due to the toxic drug crisis2.
Unregulated drug toxicity is currently the leading cause of death in British Columbians between the ages of 10 and 59, accounting for more deaths than homicides, suicides, accidents, and natural diseases combined2. Fentanyl, a synthetic opioid, has been detected in more than 85% of these unregulated drug deaths3 and is the leading cause of overdose deaths in Canada2.
[1] Overdose Prevention and Response: Guidelines for B.C.’s Post-Secondary Sector. August 2024. Covid-19 Go-Forward | Guidelines for B.C.’s Post-Secondary Sector - June 2021 (gov.bc.ca)
[2] 192 British Columbians lost to toxic drugs in March 2024: BC Coroners Service. BC Gov News
[3] More than 2,500 lives lost to toxic drugs in 2023. BC Gov News
Frequently Asked Overdose Questions
Image Source: Respond to Overdose
Opioids are drugs that are often used in medicine to treat pain. Common examples include fentanyl, oxycodone (Oxycontin, Percocet, Oxycocet, etc.), codeine, morphine, methadone, hydromorphone (Dilaudid), heroin, and others.
Fentanyl is a synthetic opioid that is extremely potent – it is 100 times more potent than morphine – and just a tiny amount of fentanyl, equivalent to three grains of sand, is enough to cause a fatal overdose, especially in first-time users. Fentanyl is often added to illicit drugs because it can be made easily and inexpensively in a laboratory. It is highly addictive and just a small amount is needed to mimic the effects of other, more expensive, opioids such as heroin.
Carfentanil, or W-18, is also starting to be found in the illegal drug market in BC. It is up to 100 times more potent than fentanyl, and an even smaller amount, equivalent to a single grain of sand, is enough to produce a fatal overdose. And so, people using illegal drugs need to be extremely careful.

Image source: Overdose prevention | Northern Health
Symptoms of an opioid overdose can include:
- - unresponsiveness (person is not moving and/or can’t be woken up)
- - slow or not breathing (less than 12 breaths per minute)
- - abnormal sounds (person may be making choking, gurgling, or snoring sounds)
- - blue lips and nails
- - cold or clammy skin
- - tiny pupils.
Fentanyl-induced muscle rigidity (FIMR) can also be present. These symptoms include stiff muscles or unusual body positions, clenched jaw, movements that look like seizures, staring at nothing, unable to speak, standing but unable to sit down, and difficulty in providing rescue breaths (due to stiffness of throat and chest muscles). For more information regarding FIMR please visit FIMR Overdoes Resources.
- 1. Call 9-1-1 immediately and let them know that you have a suspected drug overdose. If on campus, be sure to state your exact location to the 9-1-1 dispatcher.
- 2. If on campus, dial 4-4-4-4 from any campus phone during office hours (or campus security at 250-615-9894 from 5 pm to 2 am) and let them know that you have a suspected overdose. This will allow on-campus responders to quickly begin lifesaving actions while guiding emergency services to the precise location of the incident.
- 3. Stay with the person until help arrives. If you have to leave (e.g., if you are alone and need to call for help), place the person in the recovery position (see diagram below) and return to them as soon as possible. Stay with them until help arrives.
- 4. After calling 9-1-1, follow the directions from the 9-1-1 call-taker. Follow the SAVE ME steps and give rescue breaths and naloxone if you have it and know how to administer it.
- 5. Nasal naloxone kits can be found on all campuses where automated external defibrillator (AED) machines are located, as well as in every wing of student housing.
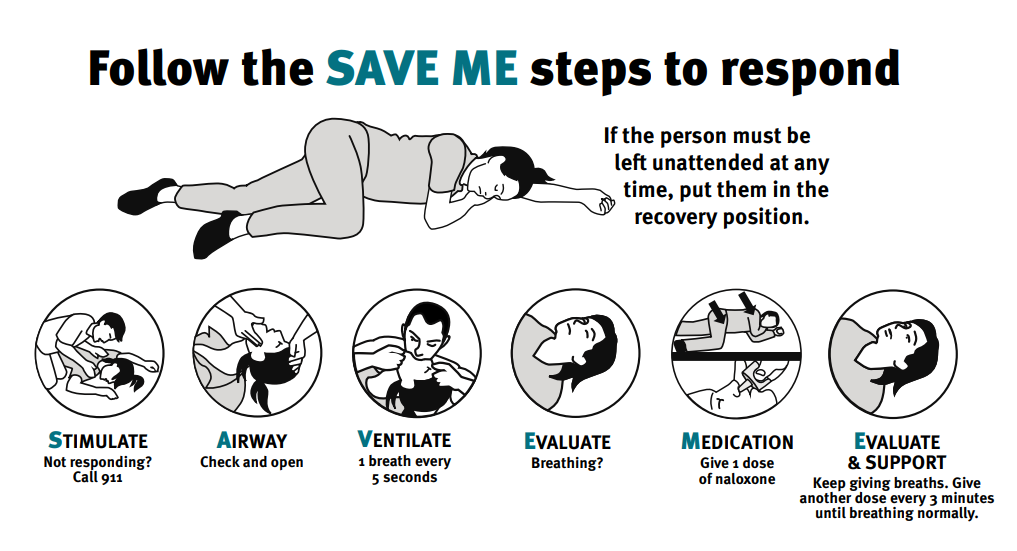
Image Source: Naloxone training
Important to Note
It’s important to note that you will NOT get in trouble for calling for help if you have also used illegal substances. The Good Samaritan Drug Overdose Act became federal law in May 2017. This law says that if you are at the scene of an overdose and you or someone else calls 9-1-1 to get medical assistance, you are not to be charged with simple possession (possession for your own personal use) of an illegal substance. You are also not to be charged for breach of probation or parole relating to simple drug possession.
Unfortunately, yes. The majority of overdose-related deaths occur in people who do not use drugs regularly and who are often unaware that they are taking fentanyl. Fentanyl has been found in more than 85% of the illegal substances tested in BC that have caused a fatal overdose. It can be added to any illegal substance, including heroin, cocaine, morphine, methadone, codeine, methamphetamine, ecstasy, crack, and others.
There is no way to tell, without testing, if fentanyl has been added to a substance. There is also a common myth that overdoses mainly occur in people who inject drugs. The reality is that 65% of people who died from toxic drugs in 2023 were smoking them, while only 14% died while injecting them.
In addition, most drug-related deaths occur in people who do not have severe drug dependencies, meaning that the majority of people who are dying from the toxic drug supply are first-time users or casual users, not regular users1.
Therefore, anyone who uses illegal substances, no matter how many times they’ve taken it and no matter what drug they think they’re taking, needs to be careful. There are no unregulated drugs that are safe.
While there is no way to guarantee safety when using illegal drugs, there are steps you can take to decrease your risk of a fatal overdose.
1. Test your drug supply for fentanyl.
Fentanyl test strips, along with instructions on how to use them, are available free of charge at the Health and Wellness Centre in Waap Amgam (House of Cedar) and in the common area in Wii Gyemsiga Siwilaawksat (Terrace Student Housing).
You can also have personal drugs tested for fentanyl at the following locations:
Terrace:
- - Terrace Health Unit (3412 Kalum St.; 250-631-4200)
- - Intensive Case Management Team (101-4450 Greig Ave.; 250-631-4647).
- The team offers fentanyl test strips. They also have a Fourier-transform infrared spectroscopy (FTIR) drug checking machine to detect the presence of other drugs in your sample.
Smithers:
- Smithers Positive Living North (3862 Broadway Ave.; 250-877-0042)
- - Specialized Mental Health and Substance Use Outreach Team (3862 Broadway Ave.; 250-643-7456)
Hazelton:
- - Hazelton Health Centre (2510 Hwy 62; 250-842-4640)
Prince Rupert:
- - Prince Rupert Health Unit (300-3rd Avenue West; 250-622-6310)
2. Don’t Use Alone or Use a Free Virtual Overdose Prevention Service
It is best not to use drugs alone and to have someone with you who can call for help if needed. If you are alone, use a free virtual overdose prevention service such as:
- - Lifeguard App (available on the App Store or Google Play)
- - Brave App (available on the App Store or Google Play)
- - National Overdose Prevention Service (1-888-688-6677).
Terrace also has access to an overdose prevention/supervised consumption site at the Northern Health Authority (Terrace Intensive Case Management Team) at 101-4450 Greig Ave.
3. Start Low, Go Slow, and Don’t Mix
Start with a small amount, especially if you are new to using drugs, if you are sick, or if it has been a while since you last used drugs, as your tolerance will be lower. Try to avoid mixing drugs, or mixing alcohol and drugs as this increases your risk of an overdose.
4. Carry Naloxone and Learn How to Use It
Make sure that you have access to naloxone when using drugs and that there is someone with you who knows how to use it.
Nasal naloxone kits are available across all campuses where automated external defibrillator (AED) machines are located, as well as in every wing of Wii Gyemsiga Siwilaawksat (Terrace Student Housing).
You can also get your own free take-home naloxone kit and training at the following locations:
Terrace:
- - Director of Student Health Services, Health and Wellness Centre room 1001a, Waap Amgam (House of Cedar)
- - Other locations: Find a Harm Reduction Site | Toward the Heart
Smithers:
- - Smithers Campus Manager, front desk
- - Other locations: Find a Harm Reduction Site | Toward the Heart
Hazelton:
- - Hazelton Community Health, 2506 62 Highway
- - Other locations: Find a Harm Reduction Site | Toward the Heart
Prince Rupert:
- - Save-On-Foods Pharmacy, 841 3rd Avenue
- - Other locations: Find a Harm Reduction Site | Toward the Heart
5. Be Informed
Although dangerous substances can be circulating at any time, the Northern Health website (Overdose Prevention | Northern Health) can alert you if there is a current overdose advisory in your area (which means that there is an increase in the number of drug poisoning/overdose events).
Please be extra cautious if there is an advisory in your area. You can also sign up for your own free text alerts by texting “JOIN” to ALERTS (253787) and following the promptsNaloxone is a medication used to rapidly reverse opioid overdoses. It works by binding to opioid receptors in the brain, displacing the opioids that are causing the overdose, and temporarily blocking their effects. It can quickly restore normal breathing in a person whose breathing has slowed or stopped due to opioids like heroin, fentanyl, or prescription painkillers.
Naloxone is available as either a nasal spray or as an intramuscular injection. Nasal naloxone kits are located across all of our campuses where automated external defibrillator (AED) machines are located, as well as in every wing of Wii Gyemsiga Siwilaawksat (Terrace Student Housing).
Free take-home intramuscular naloxone kits and training can be obtained at the Health and Wellness Centre at our Terrace campus and at the front desk at our Smithers campus. To find other locations with free naloxone kits and training close to you, please visit Find a Harm Reduction Site | Toward the Heart
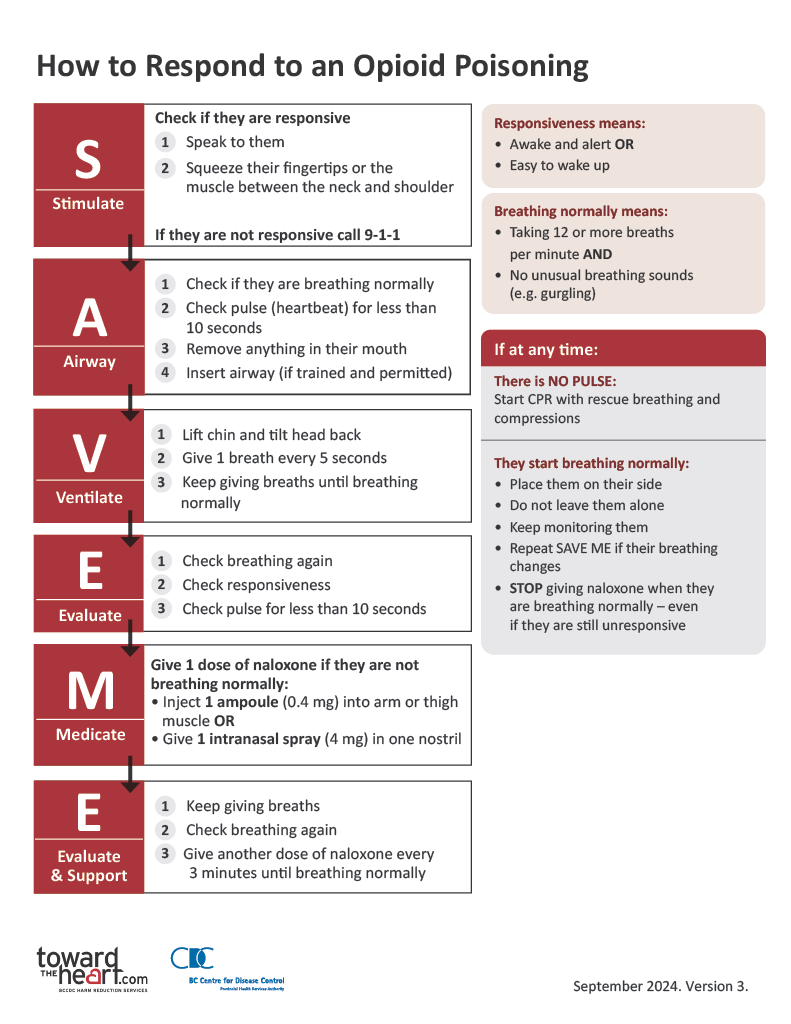
Image Source: Towards the Heart
Important Notes
- - Naloxone is safe for anyone to use, even if the person is not experiencing an opioid overdose, it will not cause harm.
- - Multiple doses of naloxone may be required for potent opioids like fentanyl.
- - Always seek medical help after administering naloxone, as it only temporarily reverses the overdose and follow up medical care will be required.
- - Although naloxone won’t work on substances other than opioids (e.g., alcohol, stimulants, and benzodiazepines), it may help if the person has taken a mix of drugs. When in doubt, use naloxone. It’s safe.
Stimulants, or “uppers”, speed the body up. They include amphetamines, crystal meth, cocaine, MDMA (Ecstasy), Ritalin/Adderall and caffeine.
Symptoms of a stimulant overdose can include:
- - rigid, jerking limbs or seizures
- - fast pulse, chest pains, and/or severe headaches
- - unconsciousness or in-and-out consciousness
- - skin feels hot and sweaty
- - anxiety, paranoia, confusion, agitation, or hallucinations.
If you suspect someone is experiencing a stimulant overdose:
- 1. Call 9-1-1 immediately and let them know that you have a suspected drug overdose. If on campus, be sure to state your exact location to the 9-1-1 dispatcher.
- 2. If on campus, dial 4-4-4-4 from any campus phone during office hours (or campus security at 250-615-9894 from 5 pm to 2 am) and let them know that you have a suspected overdose. This will allow on-campus responders to quickly begin lifesaving actions while guiding emergency services to the precise location of the incident.
- 3. Stay with the person until help arrives. If you have to leave (e.g., if you are alone and need to call for help) and the person is unconscious, place them in the recovery position and return to them as soon as possible. Stay with them until help arrives.
- 4. After calling 9-1-1 follow the directions from the 9-1-1 call-taker.
- 5. If the person is conscious, remove any objects nearby that could hurt them. Do not restrain them or put anything in their mouth. If safe to do so, move them to a calm and quiet area, away from activity and noise, and encourage them not to use any more substances. You can give them water, but don’t overhydrate. Placing cool, wet cloths on their forehead, back of neck, and armpits can help make them more comfortable.
- 6. If the person’s heart has stopped, provide cardiopulmonary resuscitation (CPR) and chest compressions or use an automated external defibrillator (AED) machine if you have one and know how to use it.
- 7. While naloxone will not reverse a stimulant overdose, it may still help if the person has taken a mix of drugs. When in doubt, use naloxone. It’s safe.
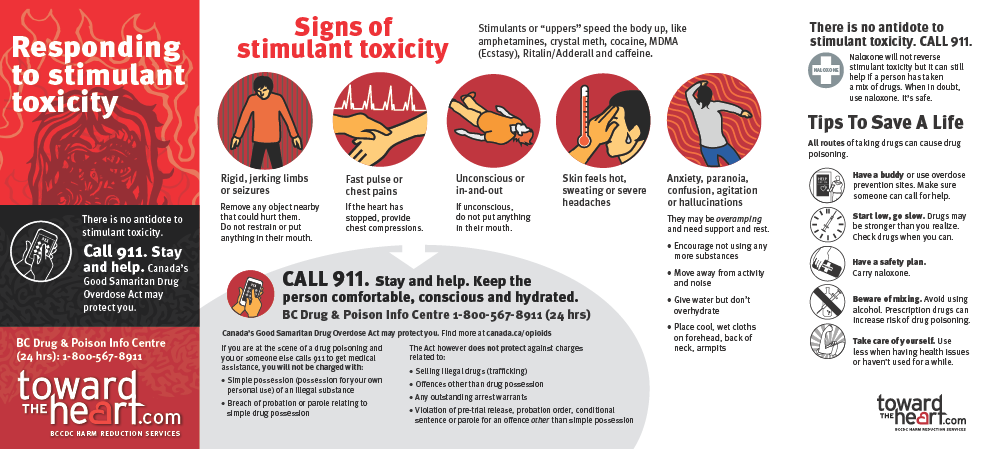
Image Source: Towards the Heart
Online Resources:
- - Toward the Heart: Toward the Heart | Toward the Heart
- - Opioid Treatment Access Line: BC Gov News
- - BC Recovery Services: BC Recovery Services – BCCSU
- - First Nations Health Authority Overdose Prevention & Harm Reduction: Overdose Prevention & Harm Reduction: Get Informed
- - BC Centre for Disease Control Harm Reduction Services: Harm Reduction Services
- - British Columbia Government Overdose Prevention and Response: Overdose Prevention and Response - Province of British Columbia
- - British Columbia Government Help Starts Here: HelpStartsHere
Terrace:
Terrace Health Unit: 250-631-7145
- - Services include opioid agonist treatment (OAT), overdose survival training, take-home naloxone kits, individual counselling, education, support, and interdisciplinary case management.
Kitsumkalum Band Council: 250-635-6172
- - Provides addiction services for Kitsumkalum band members.
- - Services include individual, family, and group counselling, as well as life skills training and referrals.
- - Prevention activities include workshops, awareness programs, and youth groups.
Terrace and District Community Services Society (TDCSS): 250-635-3178
- - Provides confidential individual, family, and group counselling; comprehensive assessment and treatment plans, referral, and prevention services; education and information on substance use and abuse; and services for those who are affected by other people’s substance abuse.
- - Services include cultural components for those who would like methods of alternative healing.
Intensive Case Management Team: 250-631-4647
- - Provides community-based team care for individuals with moderate to severe substance use problems, concurrent disorders and/or mental health illness, and who have many complex needs related to community living, including housing and income.
- - Support may include substance use counselling, housing support, access to treatment, life-skill building, and referrals to community resources, as needed.
Smithers:
Healthy Living Centre: 250-847-6234
- - Services include opioid agonist treatment (OAT), overdose survival training, take-home naloxone kits, individual counselling, education, support, and interdisciplinary case management.
Smithers Community Health: 250-847-6405
- - Services include assessment, treatment, counselling, education, and referral to community resources.
Prince Rupert:
Prince Rupert Health Unit: 250-622-6310
- - Services include assessment, treatment, counselling, education, and referral to community resources.
- - Opioid agonist treatment (OAT), overdose survival training, take-home naloxone kits, individual counselling, education, support, and interdisciplinary case management.
Friendship House Association of Prince Rupert: 250-627-1717 ExT 15
- - Provides counselling to people who are struggling with alcohol and/or drug abuse, or who are affected by someone else’s substance abuse.
Hazelton:
Mental Health and Substance Use Services: 250-842-5144
- - Services include assessment, treatment, counselling, education, and referral to community resources.
Sik-E-Dakh Health Society: 250-842-6876
- - Manages, administers, and monitors the holistic wellbeing of the members of the Glen Vowell Band on and off reserve.
- - Provides a range of health services, including substance use and addictions counselling.
Gitsegukla First Nation Health Centre: 250-849-5231
- - Services include assessment, counselling for individuals and their families, referral and self-help programs including Alcoholics Anonymous (AA) and talking circles.
Haida Gwaii:
Masset Mental Health and Substance Use Services: 250-626-4725
- - Services include assessment, treatment, counselling, education, and referral to community resources.
Haida Health Centre: 250-626-3911
- - Provides screening, assessment, individual and group counselling, and referrals for adults with addictions. Traditional teaching methods are used, including the medicine wheel.
A traumatic event can affect someone emotionally, physically, and mentally. These feelings are normal and usually pass within a few weeks. You may experience:
- - continued thoughts and images of the event
- - wanting to stay away from the scene of the event
- - difficulty concentrating
- - difficulty handling tasks or making decisions
- - feelings of guilt or wishing you had done something differently
- - nightmares and/or trouble sleeping
- - headaches or other physical reactions such as stomachaches or feeling tired all the time
- - isolating yourself from friends and/or family
- - using alcohol or drugs to numb feelings.
If you have witnessed or been through a traumatic event, it is important to take care of yourself and to reach out for help if needed. Some things that you can do include:
- - Talk to someone. Talking about it may feel uncomfortable, but it may help you feel better.
- - Avoid using alcohol or drugs as a way to cope.
- - Keep active. Physical activity is a good way to reduce stress.
- - Eat well and get enough sleep.
- - Do something you enjoy, such as a sport or hobby.
- - Use your support system. Talk to friends, family, or a counsellor.
- - A list of mental health resources can be found by visiting Mental wellness & counselling.
- - You can also make an appointment at the Health and Wellness Centre by visiting Health and Wellness Centre Bookings.
- - See your family physician if symptoms are severe or persist beyond a couple of weeks.
- - You can call the Northern Health Virtual Clinic at 1-844-645-7811 if you do not have access to a family physician.





